Introduction to Spinal Disc Tear
A spinal disc tear, also known as an annular disc tear, is a crack or rupture in the outer fibrous ring (annulus fibrosus) of one of the spinal discs that cushion the vertebrae. These discs act as shock absorbers, allowing the spine to bend and twist while protecting the vertebrae from grinding against each other.
In simple terms, think of the spinal disc as a jelly doughnut. The tough outer ring is the annulus fibrosus, and the soft, gel-like center is the nucleus pulposus. When the outer ring develops a tear or crack, the inner gel-like material can seep out, causing pain and other issues.
The impact of a spinal disc tear can be significant. The leaked inner disc material can irritate nearby nerves, leading to pain, numbness, tingling, or weakness in the affected area. Additionally, the tear can weaken the disc’s ability to cushion the vertebrae, potentially leading to further degeneration, instability, and even compression of the spinal cord or nerve roots.
Early diagnosis and treatment is important. If left untreated, a spinal disc tear can progress and lead to more severe conditions, such as a herniated disc, spinal stenosis (narrowing of the spinal canal), or even permanent nerve damage. These complications can significantly impact your quality of life and may require more extensive treatment, including surgery.
Causes of Spinal Disc Tear
Degenerative Changes
As we age, our spinal discs undergo natural degenerative changes that can increase the risk of developing a disc tear. These changes include:
Loss of disc hydration: Spinal discs are composed of a soft, gel-like center (nucleus pulposus) surrounded by a tough outer ring (annulus fibrosus). Over time, the discs lose their water content, causing them to become less flexible and more prone to cracks or tears in the outer ring.
Decreased disc elasticity: The annulus fibrosus is made up of fibrous strands that allow the disc to stretch and compress as we move. With age, these strands become stiffer and less elastic, making the disc more susceptible to tears or ruptures.
Traumatic Injuries
Sudden traumatic events, such as falls, car accidents, or sports-related injuries, can also cause spinal disc tears. The impact or force from these incidents can lead to a sudden rupture or tear in the outer ring of the disc. Even minor trauma can be enough to cause a disc tear, especially if the disc has already undergone degenerative changes.
Overuse or Repetitive Stress (Wear and Tear)
Certain occupations or activities that involve repetitive bending, twisting, or heavy lifting can put excessive stress on the spinal discs over time. This repetitive stress can gradually weaken the outer ring of the disc, making it more susceptible to tears or ruptures.
Examples of activities that may contribute to disc tears due to overuse or repetitive stress include:
Manual labor jobs: Construction work, warehouse work, or any job that involves frequent lifting, bending, or twisting can strain the spinal discs.
Weightlifting or high-impact sports: Activities that involve sudden or jarring movements, such as weightlifting, football, or gymnastics, can place significant stress on the spinal discs.
Poor posture or body mechanics: Maintaining poor posture or using improper lifting techniques can increase the strain on the spinal discs, leading to potential tears over time.
It is important to note that a combination of these factors, such as age-related degeneration and repetitive stress, can further increase the risk of developing a spinal disc tear. Adopting proper body mechanics, maintaining a healthy weight, and avoiding excessive strain on the spine can help reduce the likelihood of disc tears.
Symptoms and Diagnosis
Common Symptoms of Spinal Tears
Spinal disc tears can cause a range of symptoms, including:
Back pain: One of the most common symptoms is pain in the area of the affected disc, which can be sharp, burning, or dull and achy.
Leg pain (sciatica): If the disc tear is in the lower back, it can cause shooting pain that radiates down the back of the leg, known as sciatica. This occurs when the tear compresses the sciatic nerve.
Numbness and tingling: Disc tears can lead to numbness, tingling, or a “pins and needles” sensation in the affected area or extremities due to nerve compression.
Weakness: Patients may experience muscle weakness in the areas supplied by the compressed nerves, such as difficulty lifting the leg or foot.
Radiating pain: The pain from a disc tear can radiate to other areas, such as the buttocks, thighs, calves, or even the feet, depending on the location of the tear and the affected nerves.
The severity and location of symptoms can vary based on the specific disc level affected and the extent of the tear.
Tests Used to Diagnose Spinal Tears
While a thorough physical examination and medical history review are crucial in diagnosing a spinal disc tear, imaging tests play a vital role in confirming the diagnosis and identifying the exact location and extent of the tear.
Magnetic Resonance Imaging (MRI): MRI is considered the gold standard for diagnosing spinal disc tears and disc herniation. It provides detailed, high-resolution images of the spinal discs, vertebrae, and surrounding soft tissues. MRI scans can reveal the presence of a tear, disc herniation, or other abnormalities that may be causing the symptoms.
Computed Tomography (CT) Scan: CT scans may detect spinal disc tears, particularly when an MRI is contraindicated or unavailable. CT scans use X-rays to create cross-sectional images of the spine, allowing healthcare professionals to visualize the discs and surrounding structures. A CT discogram is the study of choice for this purpose.
In some cases, a combination of MRI and CT scans may be used to obtain a comprehensive understanding of the condition and plan appropriate treatment.
Types of Spinal Disc Tears
The tough outer layer of your spinal discs, called the annulus fibrosus, can tear in different ways. Let’s explore the three main types of tears:
Peripheral Tears: Imagine a rip on the disc’s outer rim. This is a peripheral tear, often caused by sudden impact or forceful movement. Left untreated, it can weaken the disc over time. Peripheral tears may also be known as transverse tears.
Radial Tears: These tears start deep within the disc and radiate outwards. They are more common with age-related wear and tear, but a sudden strain can also trigger them. If the tear reaches the disc’s edge, the soft inner core might bulge out, creating a disc herniation.
Concentric Tears: These are less frequent and occur within the disc’s layers, like a ring separating them. Like peripheral tears, they’re typically caused by injury.
By understanding the location and cause(s) of your tear, Dr. Lanman can create a treatment plan to address your symptoms and prevent further damage.
Non-Surgical Treatment Options
Pain Management: Over-the-counter or prescription non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen, or celecoxib can reduce inflammation and pain. Oral corticosteroids like prednisone or methylprednisolone may reduce inflammation, but these should only be used over the short-term. Epidural steroid injections deliver corticosteroids directly into the epidural space near the affected nerve roots to reduce inflammation. Lastly, nerve root blocks can deaden numb specific nerves and provide temporary pain relief.
Physical Therapy: Low-impact aerobic exercises like walking, swimming, or cycling can improve blood flow and promote healing. Core strengthening exercises support the spine and reduce stress on the discs. Stretching and flexibility exercises improve range of motion and alleviate muscle tension. Postural correction and ergonomic training may help maintain proper spinal alignment. Heat/cold therapy, ultrasound, or electrical stimulation may reduce pain and inflammation in some cases.
Lifestyle Modifications: Weight management through diet and exercise could reduce compressive forces on the spine. Proper body mechanics and lifting techniques may prevent excessive strain on the spine. Likewise, ergonomic adjustments at home or work, such as using lumbar support or adjusting workstation height, can also protect the spine. Try to avoid aggravating movements like repetitive bending, twisting, or heavy lifting. Stress management techniques like meditation, yoga, or deep breathing exercises can reduce muscle tension and improve mental wellbeing. As always, quit smoking; smoking accelerates disc degeneration and inhibits healing.
Surgical Treatment Options for Spinal Disc Tears
Indications for surgery include:
Severe, persistent pain that does not respond to conservative treatments like medication, physical therapy, or injection.
Neurological symptoms such as radiating pain, numbness, tingling, or weakness in the extremities due to nerve compression
Failed conservative treatment after an extended period (typically 6-8 weeks)
There are several surgical procedures used to treat spinal disc tears or herniated discs, including:
Discectomy: This involves removing the portion of the damaged disc that is pressing on the nerve root or spinal cord. It can be performed as an open surgery or using minimally invasive techniques like microdiscectomy.
Laminectomy: This procedure removes a portion of the lamina (bony arch) to create more space for the spinal nerves and relieve pressure caused by stenosis or disc herniation.
Foraminotomy: The surgeon enlarges the opening (foramen) where the nerve root exits the spinal canal to relieve compression from a herniated disc or bone spur.
Nucleoplasty/Plasma Disc Decompression: A minimally invasive procedure that uses radiofrequency energy to vaporize a portion of the herniated disc material and reduce its size.
Endoscopic Discectomy/Annuloplasty: A minimally invasive technique that involves inserting an endoscope and surgical instruments through a small incision to remove or repair the damaged portion of the disc.
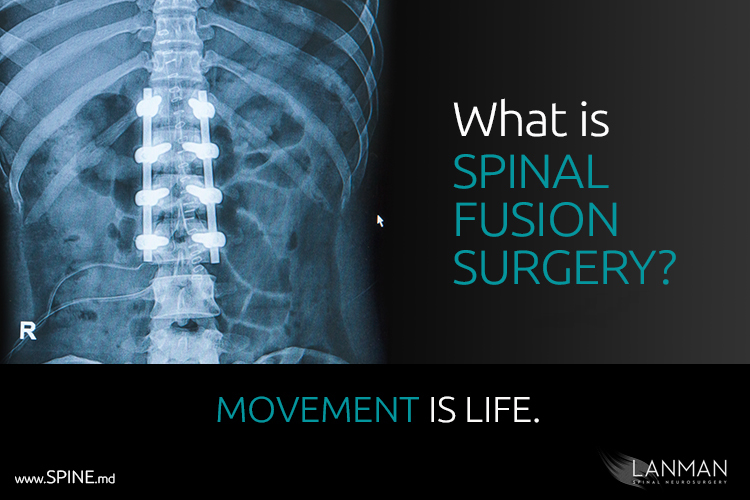
Spinal Fusion: This involves removing the damaged disc and fusing the adjacent vertebrae together using bone grafts or metal implants to stabilize the spine.
Artificial Disc Replacement: The damaged disc is removed and replaced with an artificial disc to restore height and movement between the vertebrae.
The choice of procedure depends on factors like the location and severity of the disc tear, the patient’s age and overall health, and the surgeon’s expertise. Minimally invasive techniques usually reduce recovery time and complications compared to open surgeries.
Post-Surgical Rehabilitation
Rehabilitation plays a crucial role in recovering from spinal disc surgery, regardless of the specific procedure performed. Key aspects of post-surgical rehabilitation include:
Physical Therapy: Exercises to improve flexibility, strength, and range of motion, as well as proper body mechanics
Activity Modification: Avoiding activities that place excessive stress on the spine, such as heavy lifting or high-impact exercises
Pain Management: Appropriate use of medications or other modalities to manage post-operative pain and inflammation
Gradual Return to Activity: A structured program to gradually increase activity levels and return to normal daily activities
Lifestyle Changes: Adopting healthy habits like maintaining a healthy weight, quitting smoking, and practicing good posture
The specific rehabilitation protocol will depend on the type of surgery performed, the patient’s overall health, and Dr. Lanman’s recommendations. Adherence to the rehabilitation program is essential for optimal recovery, pain relief, and prevention of future disc issues.
Prevention Strategies
Proper Body Mechanics
Maintaining Good Posture
Keep your shoulders back and avoid slouching or hunching forward
When sitting, use a small pillow or lumbar support to maintain the natural curve of your lower back
When standing for long periods, shift your weight from one foot to the other and take breaks to stretch
Lifting Techniques
Bend at the knees, not the waist, when lifting objects from the ground
Keep the object close to your body and avoid twisting your spine
Use your leg muscles, not your back, to lift heavy objects
Ask for assistance when lifting heavy or awkward items
Ergonomic Adjustments
Work Environment
Use an ergonomic chair that supports the natural curve of your spine
Position your computer monitor at eye level to avoid neck strain
Take frequent breaks to stand up, stretch, and move around
Home Environment
Use a firm mattress that supports your spine’s natural alignment
Avoid prolonged sitting or lying in positions that strain your back
Adjust the height of your work surfaces to minimize bending or reaching
Lifestyle Modifications
Maintain a healthy weight to reduce stress on your spine
Quit smoking, as it can contribute to disc degeneration
Stay active and engage in low-impact exercises like walking, swimming, or cycling
By incorporating these prevention strategies into your daily routine, you can help reduce the risk of spinal disc tears and promote overall spinal health.
Complications and Long-Term Management
Untreated or poorly managed disc tears can lead to several serious complications, including:
Nerve Damage: The torn disc can protrude and compress the surrounding nerves, leading to radiating pain, numbness, tingling, and weakness in the affected areas. Prolonged nerve compression can cause permanent nerve damage.
Chronic Pain: If the tear is not properly treated, the inflammation and irritation can persist, leading to chronic and debilitating back and/or leg pain.
Disability: Severe disc tears can significantly limit mobility and functionality, potentially leading to disability and an inability to perform daily activities or work.
Cauda Equina Syndrome: In rare cases, a large disc herniation can compress the cauda equina nerves, causing loss of bladder/bowel control and lower body weakness—this is a medical emergency requiring immediate surgical decompression
Long-Term Management
For chronic or recurrent disc tear symptoms, long-term management strategies may include:
Lifestyle Modifications
Weight management to reduce stress on the spine
Ergonomic adjustments at work and home
Low-impact exercise like swimming or cycling to strengthen core muscles
Avoiding activities that involve repetitive bending, twisting, or heavy lifting
Pain Management
Over-the-counter or prescription anti-inflammatory medications
Epidural steroid injections to reduce inflammation and pain
Physical therapy and stretching exercises
Surgical Options
Minimally invasive procedures like microdiscectomy or nucleoplasty to remove or shrink the protruding disc material
Artificial Disc Replacement
Consistent follow-up with a spine specialist like Dr. Lanman is crucial for monitoring the condition and adjusting the treatment plan as needed. Adopting preventive measures like maintaining good posture, using proper lifting techniques, and staying active can help reduce the risk of recurrence or worsening of disc tears.